Written by Henry Lin and Edited by Catherine Zhang
Imagine a warm day where you decided to take a dip in a nearby lake to cool yourself off. As you splash around full of carefree joy, you would never have expected to be lying on a hospital bed two weeks later at the brink of death. Unbeknownst to you, the waters you had jumped into contained multitudes of single-celled organisms called amoebae that are now slowly consuming your brain.
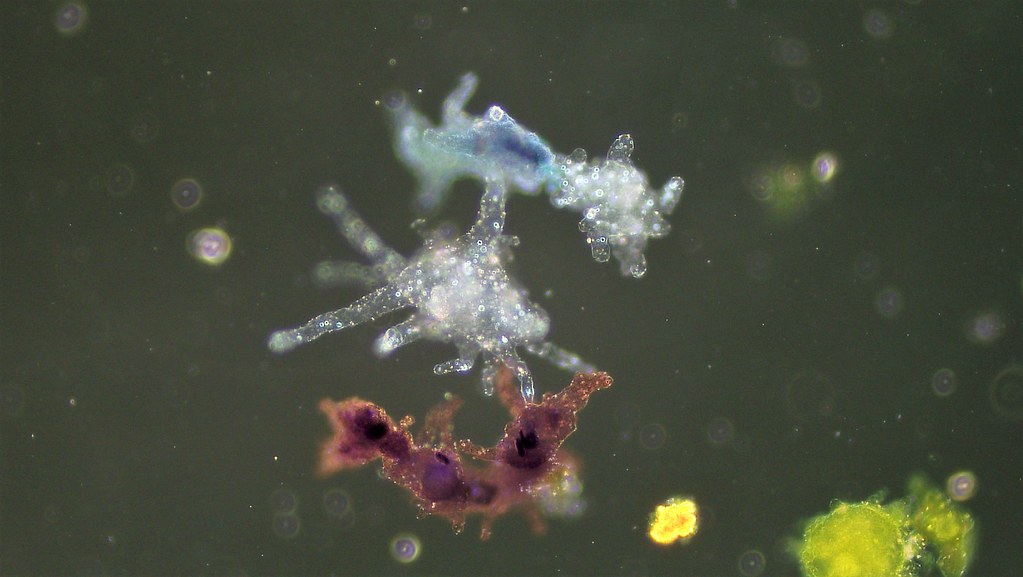
Many are probably familiar with Hollywood’s depiction of brain-eating zombies, but the idea of microscopic organisms taking on the same role seems highly implausible; thus, it escapes the minds of those who unwittingly fall prey to them. Such organisms are amoebae: single-celled eukaryotes, which are cells with DNA enclosed within a membrane-bound nucleus, that live virtually everywhere on Earth—the soil, sand, or water—with a versatile diet that ranges from bacteria and algae to small worms and human cells [1]. While Hollywood’s zombies are only works of fiction, certain species of amoebae, such as Naegleria fowleri and Acanthamoeba, are real and can cause deadly infections by functioning very similarly to zombies: eating brains.
Naegleria fowleri and Acanthamoeba both live within bodies of warm water, but they cause infections in different ways. Infections by Naegleria fowleri occur when there is an “accidental inhalation of infected water up the nose that allows the amoeba to travel across the cribriform plate, which separates the nose and brain” [2]. Once Naegleria fowleri reaches the brain, it consumes brain cells for sustenance, causing Primary Amoebic Meningoencephalitis (PAM) [3]. PAM is a brain infection with symptoms similar to meningitis, including the following: headaches, fevers, nausea, and seizures [3]. On the other hand, Acanthamoeba causes infections by entering through cuts in the skin, where it travels through the bloodstream to different parts of the central nervous system, consuming brain cells and causing Granulomatous Amoebic Encephalitis (GAE) [4]. GAE occurs when both the brain and spinal cord become infected, and results in symptoms different from PAM, including loss of coordination, loss of muscular function, and increased sensitivity to light [5].
Unfortunately, Naegleria fowleri and Acanthamoeba infections are usually fatal. Although rare, PAM caused by Naegleria fowleri has a 98% mortality rate, with less than 5 survivors in the past half-decade [4]. Those that develop GAE face a 95% mortality rate [2]. In addition to the high mortality rates, Acanthamoeba species can also host Multidrug-Resistant (MDR) Bacteria [4]. In other words, certain antibiotic-resistant bacteria are able to attach themselves to Acanthamoeba and increase in population. Since these bacteria are resistant to antibiotics, they can grow unhindered into dangerous infections when exposed to humans.
Global warming plays a large role in increasing the danger and occurrence of amoebic infections. Naegleria fowleri and Acanthamoeba amoebae thrive and become trophozoite (infectious) in warm temperatures [4]. As the global temperature rises, Naegleria fowleri and Acanthamoeba will become active for longer periods of time, which supports the production of MDR Bacteria, further increasing the danger humans face when exposed to free-living amoebae.
When someone is infected by Naegleria fowleri or Acanthamoeba, they usually recover if they are treated right away [5]. Current medication and treatment options are limited due to a lack of clinical trials, but recently, the anti-leishmania drug Miltefosine was shown to be an effective treatment against PAM [3]. As more treatment plans are developed, the main challenge is identifying the infections as soon as possible.
In order to combat the fatal nature of amoebic infections, the most important step is to inform people about the dangers of entering warm bodies of water [6]. Especially since most reported cases are the result of people swimming or diving in warm bodies of freshwater, such as lakes and rivers [3]. New forms of medication need to be developed in order to treat the infections, since most current ones are unable to effectively cross biological barriers into the brain without harming the individual’s cells [2]. Finally, there needs to be more funding put into the research and collection of epidemiological data on amoebic infections, as well as the sharing of the same data between researchers and physicians to ensure up-to-date treatments [7].
References:
[1] Vidyasagar, Aparna. “What is an Amoeba?” Live Science, Future US Inc, 2016, www.livescience.com/54281-amoeba-definition.html.
[2] Khan N. A., Ong Y. Y. T., Siddiqui R. (2017). Targeting Brain-Eating Amoebae Infections. ACS Chemical Neuroscience, 8: 687-688.
[3] U.S. Department of Health and Human Services. “Parasites — Naegleria fowleri — Primary Amebic Meningoencephalitis (PAM) — Amebic Encephalitis.” Centers for Disease Control and Prevention, 2017, www.cdc.gov/parasites/naegleria/index.html.
[4] Baig, M. A. (2019). Global Warming Favors Pathogenicity of the Brain-Eating Amoebae. Anti-Infective Agents in Medicinal Chemistry, 17:2-3.
[5] U.S. Department of Health and Human Services. “Parasites — Acanthamoeba — Granulomatous Amebic Encephalitis (GAE); Keratitis.” Centers for Disease Control and Prevention, 2017, www.cdc.gov/parasites/acanthamoeba/index.html.
[6] Pervin, Najwa and Vidya Sundareshan. (2019). Naegleria. StatPearls Publishing, published online.
[7] Khan N. A., Anwar A., Siddiqui R. (2017). Future Priorities in Tackling Infections Due to Brain-Eating Amoebae. ACS Chemical Neuroscience, 8: 2355-2355